The two-year Ebola epidemic which laid waste to communities across west Africa and killed more than 11,000 people is due to be declared over Thursday with Liberia expecting the all-clear.
The worst outbreak of the tropical pathogen in history has devastated health services and wrecked the economies of the hardest hit nations since it emerged in southern Guinea in December 2013.
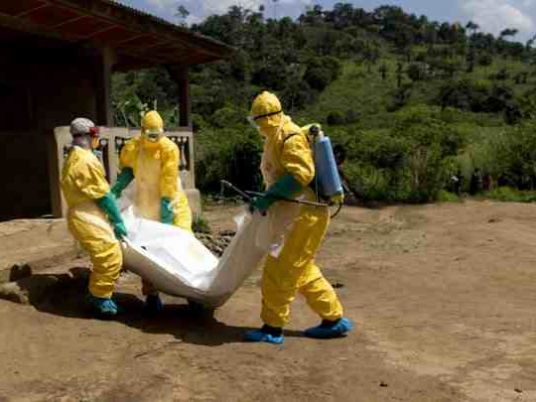
At its height, the epidemic cut a swathe through the capital cities of Guinea, Liberia and Sierra Leone, with bodies piling up in the streets and overwhelmed hospitals recording hundreds of new cases a week.
WHO said Thursday's announcement in Geneva will "mark 42 days since the last Ebola cases in Liberia were tested negative". The announcement was previously scheduled for Friday, and no reason was given for the change.
"We will remain careful and keep calling on the population to take the necessary measures in preventing reoccurrence," said Francis Karteh, Liberia's chief medical officer and major figure in the response to the epidemic.
Liberia, hardest hit in the outbreak with 4,800 deaths, discharged its last two cases — the father and younger brother of a 15-year-old victim — on December 3.
It was the last country affected by an outbreak infecting almost 29,000 people and claiming 11,315 lives, according to official data which most experts accept represents a significant underestimate.
The patients' recovery triggered a 42-day countdown — twice the incubation period of the virus — before Liberia can be declared free of transmission for a third time.
Ebola can fell its victims within days, causing severe fever and muscle pain, weakness, vomiting and diarrhoea. In many cases it shuts down organs and causes unstoppable bleeding.
The virus is spread through close contact with the sweat, vomit, blood or other bodily fluids of an infected person, or the recently deceased.
Aggressive spread
Liberia was first declared free of human-to-human transmission in May, only to see the fever resurface six weeks later, It was officially credited with beating the epidemic for a second time in September before another small cluster of cases emerged.
The virus spread aggressively from "patient zero", a Guinean infant who became the first victim, into Liberia and then Sierra Leone, quickly notching up more deaths than all other outbreaks combined.
Sporadic cases were also registered in Mali, Nigeria and Senegal as deaths mounted at a dizzying rate, igniting fears in Europe and elsewhere of a virus that transgressed borders and national controls.
The epidemic devastated the economies of the worst-hit countries, as crops rotted in the fields, mines were abandoned and goods could not get to market.
Strong recent growth has been curtailed in Guinea and while Liberia has resumed growth, Sierra Leone is in a severe recession according to the World Bank, which has mobilised $1.62 billion for Ebola response and recovery efforts.
"Ebola has reduced me to a pauper, as many of my creditors were foreigners, mainly Nigerian nationals," said textile dealer Mohamed Sow, one of numerous entrepreneurs interviewed by AFP in Sierra Leone this week who have described being ruined by the epidemic.
Existential threat
"They owed me millions and they left Freetown when the Ebola virus was raging."
During the two months of peak transmission in August and September 2014, Liberia's capital Monrovia was the setting for some of the most harrowing scenes from the outbreak.
The largest Ebola unit ever built opened there with 120 beds in August 2014 but was immediately overwhelmed, with staff forced to turn patients away at its gates, despite more than doubling its capacity.
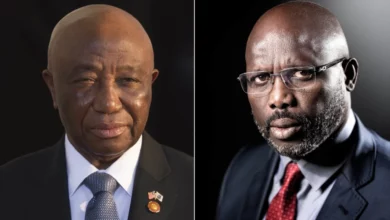
Liberian Defence Minister Brownie Samukai told a meeting of the UN Security Council that the country was facing "a serious threat to its national existence".
At the time, more than 400 new cases were being reported each week, with uncollected and highly infectious bodies piling up in the streets of Monrovia, a sprawling, chaotic city at the best of times.
Schools remained shut after the summer holidays, unemployment soared as the formal and black market economies collapsed, clinics closed as staff died and non-emergency healthcare ground to a halt.
Amid the horror, one case stood out as uniquely cruel.
In the quarantined hamlet of Ballajah, 150 kilometres (90 miles) from the capital, 12-year-old Fatu Sherrif was locked into her home with her dead mother as panicked neighbours fled to the forest.
Her cries could be heard for several days by the few who had stayed in the abandoned village before she died alone, without food or water.
The international community came under fire for a response that saw west African states treated as pariahs.
But that all changed when aid workers started falling ill and going home for treatment, resulting in the first-ever domestic infections outside of Africa — two in the United States and one in Spain.
From a position of indifference, the West rallied to the cause, sending thousands of troops and medics to Africa in 2014 and developing possible treatments and vaccines, many of which are still being tested.